Introduction
People are increasingly seeking answers to their problems online and those with neuromusculoskeletal pain are no exception! Searchers who chose virtual physical therapy rated their satisfaction level and results comparable to in-person therapy. There has been a 45% increase around the world in disabilities due to neuromusculoskeletal dysfunctions in the past 10 years and the trend is expected to continue.
Waiting weeks for care
The internet has become the first stop to gather information for those who are suffering from pain or illness and it makes sense! The traditional medical system has been spread too thin for years and it is only getting worse. The average time it takes to see a primary care physician is 24 days. To see a medical specialist is even longer at an average of 53 days! For someone suffering from pain, this waiting period can lead to additional stress, anxiety, and depression, as well as negatively affect overall outcomes.
Table of contents:
What is Physical Therapy?
Why is Physical Therapy important?
Physical Therapy’s Beginning
Modern Physical Therapy
Emerging trends and advancements
Virtual Physical Therapy
What does the research say about virtual Physical Therapy?
Who is appropriate for virtual Physical Therapy?
Key to success with Physical Therapy
Table of contents:
What is Physical Therapy?
Why is Physical Therapy important?
Physical Therapy’s Beginning
Modern Physical Therapy
Emerging trends and advancements
Virtual Physical Therapy
What does the research say about virtual Physical Therapy?
Who is appropriate for virtual Physical Therapy?
Key to success with Physical Therapy
Introduction
People are increasingly seeking answers to their problems online and those with neuromusculoskeletal pain are no exception! Searchers who chose virtual physical therapy rated their satisfaction level and results comparable to in-person therapy. There has been a 45% increase around the world in disabilities due to neuromusculoskeletal dysfunctions in the past 10 years and the trend is expected to continue.
Waiting weeks for care
The internet has become the first stop to gather information for those who are suffering from pain or illness and it makes sense! The traditional medical system has been spread too thin for years and it is only getting worse. The average time it takes to see a primary care physician is 24 days. To see a medical specialist is even longer at an average of 53 days! For someone suffering from pain, this waiting period can lead to additional stress, anxiety, and depression, as well as negatively affect overall outcomes.
There is no doubt the COVID-19 pandemic was a huge catalyst for the exponential growth in virtual physical therapy. “Necessity is the mother of innovation.” But is this movement into the virtual realm when it comes to physical therapy good? Let’s first look at what physical therapy is and how it started…
What is physical therapy?
According to guidelines published by the American Physical Therapy Association, physical therapy should be defined as the examination, treatment, and instruction of persons to detect, assess, prevent, correct, alleviate, and limit physical disability and bodily malfunction. Physical therapists are movement experts who optimize quality of life through prescribed exercise, hands-on care, and patient education. (APTA)
Why is physical therapy important?
It is the human body’s job to heal itself after an injury or illness. Even when a surgeon performs a procedure to repair, remove, or reposition bodily tissue it is still the body’s job to then heal itself! This is an autonomic response meaning the body does it automatically! BUT once the body’s illness has resolved or its tissues have healed does movement and/or function spontaneously restore? This is where Physical Therapy comes in….
Physical therapy is important because it:
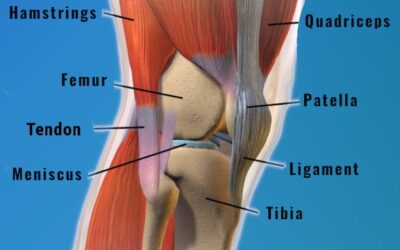
Ensures that the right amount of stress is applied to the body’s tissue at the appropriate stages of healing. Appropriate loading of musculoskeletal tissue during recovery not only promotes healing, but also strengthens the bone, muscle, tendon, and/or ligament involved.
Ensures movement is restored. Although the body heals itself it is the rehabilitation process that makes sure the injured area regains its range of motion, strength, and balance. This will also reduce compensatory movement which usually leads to future problems elsewhere in the body.
Prevents reinjury. Bones, muscles, tendons, ligaments, cartilage, and even the spine’s intervertebral discs respond and adapt to the stress applied to them! Physical Therapy assists with making the body resilient to reinjury through an appropriate progression of exercise.
Empowers patients to reach their goals. It’s hard to reach a goal if you don’t have a plan. Physical Therapy will guide someone through their specific stages of recovery to maximize outcomes!
Restores functional independence. Physical therapy is an integral part of the rehabilitation process for people who suffer from neurological disease or events and amputation. Whether re-learning how to walk, or developing adaptive strategies, physical therapy can significantly improve the quality of life for these patients.
Prevents falls. Falls are a huge problem especially in the elderly. According to the CDC, falls cause high mortality rates in individuals over the age of 85. Physical therapy helps improve balance strategies and provides safety education.
Can help avoid surgery. Pre-physical therapy or “Prehab” is a term used when physical therapy is prescribed before surgical interventions to enhance post-operative results. The better someone is moving before surgery, the better someone is going to move after surgery! Many times pre-physical therapy can even result in the avoidance of surgery altogether.
Physical therapy’s beginnings
The roots of physical therapy can be traced back to ancient times! Ancient Persia, China, and Egypt all have writings that describe the use of exercise, movement, and massage for ailments. Hippocrates (460–385 BC), the father of medicine, was the first physician to describe using exercise after spinal manipulations and manual therapy techniques to treat illness and relieve pain.
Hippocrates quotes
“That which is used develops, and that which is not used will waste away. If there is any deficiency in exercise the body will become liable to disease, defective in growth, and age quickly.”
”If we could give every individual the right amount of nourishment and exercise, not too little and not too much, we would have found the safest way to health.”
The physical therapy we know today began to take form in the 18th century with Per Henrik Ling a Swedish physiologist, gymnastics instructor, and expert fencer. He founded the Royal Central Institute of Gymnastics in the year 1813. The institute provided massage, manipulation, and exercise to treat injuries and illnesses. It wasn’t until 1851, the term “Physiotherapy” first appeared in a German article written by Dr. Lorenz Gleich, a military physician from Bavaria. In 1887, Sweden’s National Board of Health recognized physiotherapy (physical therapy) as a viable health practice. Soon nearby countries in Europe also established physical therapy as an accepted treatment method.
In America, “rehabilitative therapy” was mainly provided to injured World War I soldiers by reconstruction aides from 1917-1918. The Polio epidemic contributed to the increased demand for physical therapy and led to advancements in treatment techniques. In 1921 Mary McMillan established the American Women’s Physical Therapeutic Association and she became known as the “Mother of Physical Therapy.” The organization’s name was later on changed to the American Physical Therapy Association (APTA).
Modern physical therapy
Physical therapy was only performed in hospitals until the 1950’s. It wasn’t until the late 1950s that physical therapists started treating their patients beyond hospitals and in the outpatient setting. The APTA formed an Orthopedic Section In 1974. It was for the physical therapists who had specialized in medicine dealing with the correction of deformities of muscles and bones, as well as joints, ligaments, and tendons.
The practice of Physical therapy continued to progress in the 1980’s with the development of computers and technology. Modality devices such as electrical stimulation and ultrasound machines became more prevalent in the field to augment exercise and manual therapies. Many of these devices are still used in Physical Therapy clinics today!
During the next three decades, the profession continued to grow substantially and diversified. Specialties such as cardiopulmonary physical therapy, neurological physical therapy, sports physical therapy, geriatric physical therapy, pediatric physical therapy, pelvic-floor physical therapy, and vestibular physical therapy were recognized by APTA, along with orthopedics.
Today physical therapists have a role in the treatment plan of almost every individual who enters the medical system. Physical therapists are in hospitals, skilled nursing and assisted living facilities, out-patient clinics, and even go to the home of patients. Physical therapy has evolved throughout time into a multitude of techniques with specialized applications, but its principles have been around for a millennia!
Professional advancements and emerging trends
Direct Access. All 50 states, Washington, D.C., and the U.S. Virgin Islands enjoy some form of direct access to physical therapist services. However, provisions and limitations vary among jurisdictions. Direct access means an individual can obtain physical therapy services without a prescription or referral from a physician. Since 2016 all graduating physical therapists must have a doctorate level degree (DPT) which helped the profession gain this level of autonomy. Advocates say removing the need for a physician referral will reduce delays in care. Speedier care means lower costs, improve functional outcomes, and reduced frustration for patients seeking physical therapy treatment.
Dry needling. Dry needling is a skilled intervention where a thin filiform needle penetrates the skin. This treats the underlying muscles for the management of neuromusculoskeletal pain and movement dysfunction. The procedure is performed by a physical therapist who has met certification requirements including expertise in anatomy.
IASTM. Instrument assisted soft tissue mobilization (IASTM) is a manual therapy technique. Metal or plastic tools are used to induce an erythemic response to targeted tissues thus promoting tissue healing.
Cupping. Cupping is a very old technique that only recently has been added to the physical therapy toolbox. Cups are placed on a specific treatment area using a wet or dry technique. Inside the cup, a vacuum or suction force pulls the skin upward. This suction force expands and breaks open tiny blood vessels under the skin. This trauma promotes a healing response and is thought to release toxins for the lymphatic system to clear.
Blood flow restriction. Blood flow restriction (BFR) training uses a tourniquet-style cuff on the proximal aspect of a limb. The cuff is inflated to a pressure that occludes venous flow yet allows arterial inflow during exercise. Data confirms BFR training can promote muscle strength and hypertrophy with low load exercises. This technique is extremely useful in physical therapy. Patients may be restricted by a post-operative protocol or may be unable to tolerate high-load exercise which is usually necessary for increasing muscle strength and hypertrophy.
Virtual physical therapy
The concept of remote healthcare isn’t new. In the 1880’s the telephone was used by physicians to prevent unnecessary visits. But, in 2020 the COVID-19 pandemic made remote healthcare a necessity for many. It seemed like overnight patients in all disciplines of the medical system had to learn how to participate in “telehealth.” In the field of physical therapy, it was now the therapist’s job to evaluate patients without the use of one of their most treasured tools…their hands.
This demanded that physical therapists come up with new ways to examine movement and develop an effective treatment plan. Many believe the pandemic just accelerated an inevitable transition into virtual healthcare. A landmark publication, Crossing the Quality Chasm, stated, “information technology must play a central role in the redesign of the health care system if a substantial improvement in quality is to be achieved.”
Virtual physical therapy can come in different packages.
The first is a one-on-one consultation through a technology platform where a physical therapist will evaluate an individual’s reported symptoms and observe movement, as well as run necessary special tests. They will then develop a plan which may include exercise, doing it yourself manual therapies, modalities (ice and or heat), and adaptive or bracing equipment. They also may plan a few follow-up appointments to make sure the patient is making progress towards their specific goals.
Another option is purchasing an online physical therapy plan or protocol specific to a common diagnosis. For example, a do it yourself step by step guide to treating plantar fasciitis, runner’s knee, or tennis elbow. This plan will usually include the appropriate exercises with how many sets and repetitions, exercise progressions, etc. It may use pictures and/or videos for exercise descriptions.
To add, there is also a wealth of information, valuable and invaluable, on social media platforms that are free and readily available. These sources usually present themselves as, “fix your back in five steps” or “resolve your headaches with this exercise”. Since this type of information is free and easily obtained, consumers should be mindful that this may not necessarily be the comprehensive fix to the issues for which they are seeking aid.
Is virtual physical therapy effective? What does the research say?
The research overwhelmingly supports the effectiveness and efficacy of telehealth physical therapy.
Patient satisfaction rates were comparable to in-person physical therapy except for scheduling appointments and individualized time with the therapist where the data shows patients favored VIRTUAL services.
Research shows that physical therapy outcomes are similar between virtual and in-person for certain diagnoses.
Telehealth is a proven and effective alternative for individuals who are unable to access in-person healthcare services for the management of many musculoskeletal conditions.
When it comes to healthcare costs to the consumer studies determined those who utilize virtual physical therapy had an average savings of 13%.
Who is appropriate for virtual physical therapy?
Virtual physical therapy is great for those who have time constraints due to work or family, as well as financial limitations that make going to a physical therapy clinic impossible. Although virtual physical therapy is appropriate for most of the population some factors that should be considered when determining if this type of healthcare is right for you.
Do you have reliable and convenient internet access? This is pretty much a must-have to participate in virtual physical therapy.
How is your technological literacy? This isn’t so much of a “must” as the programs have become significantly easier to navigate. Most of the time all you have to do is click on a link. However, we all know some will still have an issue and if so virtual physical therapy may not be for you.
Are you self-motivated? Most of the time telehealth appointments are less frequent than in person physical therapy, or in some cases, virtual physical therapy may not involve any formal appointments. Therefore, the patient must hold themselves accountable to comply with prescribed therapeutic interventions.
Do you need hands-on treatment? There are some manual techniques that can be performed on yourself with the right training and equipment, but there are times when someone requires the skilled hands of a physical therapist.
Are you at risk of falling? A physical therapist is thoroughly trained in proper “guarding” skills which means protecting a patient from falling during treatment. If you are at a high fall risk then you will require the skills of a present physical therapist to prevent a fall as you challenge your balance, walking, etc.
Keys to success with any physical therapy
Whether a person decides to undergo in-person physical therapy or participate in virtual physical therapy there are a few things that are key to making your treatment a success:
Patient buy-in: This is a term used when the patient has been sufficiently educated on their specific impairments. And understands how physical therapy interventions are going to help. They believe the plan is going to work! This helps with promoting the next key.
Compliance: Physical therapy interventions aren’t magic. It is using the principles of exercise to restore motion, increase strength, improve balance, and reduce pain. We all know exercise works, but only if you do it! You must be committed and consistent!
Give it time: Along with consistency and compliance with exercise, we also know change takes time. Tissue healing takes time and the changes exercise induce takes time.
The physical therapist can be crucial in causing positive short term results. For example, a decrease in pain after a modality, or an increased range of motion after manual therapy. However, real life positive change occurs when the patient is ACTIVE in their recovery!





0 Comments
Trackbacks/Pingbacks